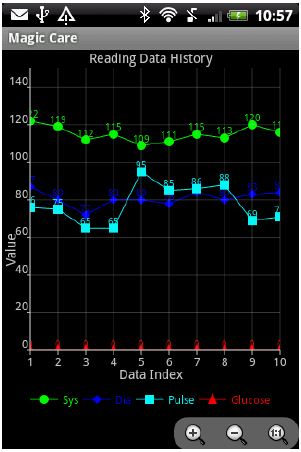
Generated Chart | ||
 |
Unite in the fight against noncommunicable diseases
Noncommunicable diseases or NCDs like heart attacks and strokes, cancers, diabetes and chronic respiratory diseases — kill about three in five people worldwide (63 percent), and cause great socioeconomic harm in all countries, particularly in developing countries like Bangladesh. Every year, 9 million people die too young from NCDs (under the age of 60). But implementing cost-effective interventions that reduce risk factors for NCDs will contribute up to two-thirds of the reduction in premature mortality. Global leaders urged to set a new international agenda on NCDs to take action against the epidemic, save millions of lives and enhance development initiatives.
While the international community has focused on communicable diseases such as HIV/AIDS, malaria and tuberculosis, the four main non-communicable diseases have emerged relatively unnoticed in the developing world and are now becoming a global epidemic. However, such diseases could be significantly reduced and prevented.
Four types of noncommunicable diseases — cardiovascular diseases, diabetes, cancers, and chronic respiratory diseases — make the largest contribution to mortality in the majority of countries. These four NCDs are largely preventable by means of interventions that tackle four risk factors for NCDs: tobacco use, unhealthy diets, physical inactivity, and harmful use of alcohol.
The impact of non-communicable diseases can be prevented with an approach that incorporates cost-effective, population-wide health-care interventions to address risk factors, known as public health “best buys”, and primary health-care measures to treat those who have contracted or are at high risk of contracting such diseases. The widespread implementation of such interventions, which require modest investment, can lead to quick gains in counteracting the effects of non-communicable diseases.
The best buys for population-wide interventions include tobacco-control measures, including raising taxes and bans on advertising and smoking in public places; raising taxes on alcohol and enforcing bans on alcohol advertising; reducing salt intake; replacing trans-fats in foods with polyunsaturated fats; promoting public awareness about diet and physical activity; and delivering hepatitis B vaccinations. Primary health-care interventions include counselling, multi-drug therapy and screening and early treatment for cervical and breast cancers.
The burden of non-communicable diseases in low- and middle-income countries goes beyond the fact that those countries are home to the world’s largest populations. Unplanned urbanisation, ageing populations and the globalisation of trade and product marketing, particularly for tobacco, alcohol and food, have led to a rise in the risk factors of such diseases.
The lack of healthcare capacity and social protection systems in lower-income countries means that non-communicable diseases are more likely to cause people to become sick and die from them at earlier ages. The knowledge and technology to fight the onset and effects of non-communicable diseases already exist. It is the high time to act to save future generations from the health and socio-economic harm of such diseases.
Source: World Health Organisation (WHO)
Battling the world’s deadliest diseases
The world’s deadliest and most debilitating chronic diseases are about to be propelled to the top of the global health agenda.
The foremost health-care decision-makers from across the globe will gather on Sept. 19 at United Nations Headquarters in New York for a first-of-its-kind global health assembly to address the rapidly escalating mortality rates being inflicted by non-communicable diseases (NCDs), such as cardiovascular disease, diabetes, cancer and lung disease.
The 2011 high level meeting on the prevention and control of NCDs recognizes that these illnesses pose a global health-care challenge unlike any ever faced.
Consider this:
• Every day more than 100,000 people die of an NCD worldwide.
• In 2008, more than six out of 10 people died from an NCD. By 2030, that number will be more than seven out of 10.
• By 2030, nearly three out of four people who die will do so as a result of an NCD.
NCDs have surpassed communicable diseases as the world’s primary health concern. The sheer scope of the problem calls for solutions related to prevention, diagnosis and treatment far beyond what any one government or institution can enact and requires a highly coordinated effort by governments, academia and the private sector.
NCDs represent an extraordinary global drain on health-care resources:
• NCDs account for roughly 75 cents of every dollar spent on health care in both advanced and developing economies.
• In developing countries, nearly 50 per cent of NCD deaths occur among people in their most productive years (before age 70) accounting for more than $1 trillion in lost income.
• Productivity losses associated with workers with chronic disease are as much as 400 per cent more than the cost of treating chronic disease.
While nearly 80 per cent of NCD deaths in 2008 occurred in low- and middle-income countries, the truth is that even the most advanced nations and economies are not immune to the deadly impact of NCDs. In Canada, chronic diseases account for approximately 85 per cent of all deaths.
Furthermore, in 2005, the World Health Organization projected that over the ensuing 10 years (from 2005 to 2015) more than two million Canadians would die from a chronic disease, deaths from chronic disease would increase by 15 per cent and, most markedly, deaths from diabetes would increase by 44 per cent.
In Canada, the only way we are going to meet the needs of an aging population and effectively address the challenge of NCDs is to make the system more efficient.
Governments and health-care providers must challenge the conventional thinking that investing in health care is a zero-sum game. We need to get our heads around the idea that investments in innovation — whether new software, medical technology or best practices — will save money over conventional approaches in the long run.
Through investments in innovations, such as remote monitoring, the creation of an artificial pancreas and electronic medical records, the health-care system can significantly decrease the time spent in emergency rooms, shorten recovery times, lessen the reliance on pharmaceuticals, and improve the dissemination of patient information among health-care professionals. By focusing on both efficiencies and innovation we will improve the overall patient experience in Canada.
Health policy analyst Ted Ball points out that “health-care system costs can be reduced by 30 per cent by implementing more efficient processes that maximize the benefit to patients and increase quality of care.” In my mind, that’s a conservative estimate.
The outcome of the UN’s high level meeting will be a plan of action and a commitment from heads of government for a coordinated global response to NCDs. However, as UN Secretary-General Ban Ki-moon noted earlier this year, government intervention alone simply isn’t enough. The scope of this global health challenge calls for solutions far beyond the ability of any single institution or the public sector to implement.
The main thrust of the NCD effort is to harness global efforts to drive solutions for the lesser-developed countries. We all need to work toward a world where every person suffering from chronic disease who could benefit from diagnostic, therapeutic and disease management solutions will get them.
Hopefully, the 2011 NCD meeting will be a watershed moment in the way the world addresses the world’s leading killer — non-communicable diseases.
Neil Fraser is Co-Chair of the Ivey Centre for Health Innovation/Leadership and President of Medtronic of Canada Ltd.
Mobile Application for TeleHealth Systems, MagicCare for Android Screenshorts
Installed MagicCare Application | Main Screen | |
 | 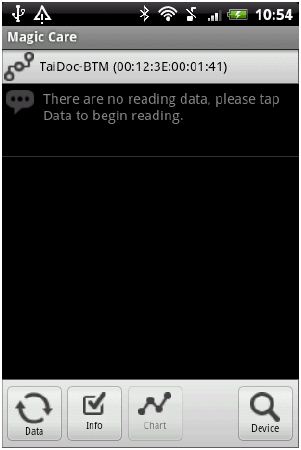 | |
Device Selection | Querying Device Information | |
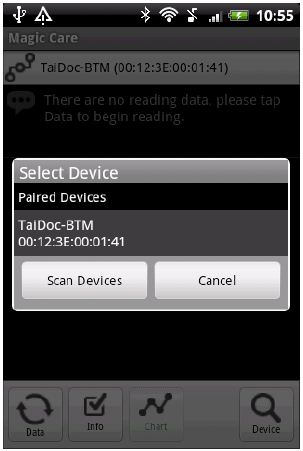 | 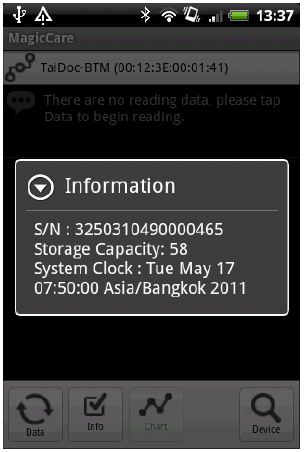 | |
Data Reading | Reading Data List | |
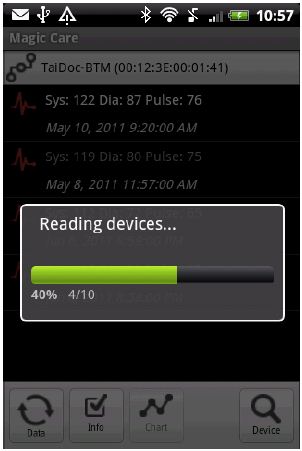 |  | |
Preventive Care - Telehealth systems for High Blood pressure and Glucose





It would be triggered automatically when the data is out of alert level. It can be sent to patient, doctor and patient family members.



Patient measure their blood pressure and glucose level with ease
- The device record and store the information into memory
- The device is easy to carry and use
- It has approvalfrom FDA/CE

- Glucose and blood pressure meter
- Mobile computer
The store information of patient historical blood pressure and glucose level can be uploaded by the smart phone, computer with ease and wirelessly

Medical professional, doctors or nursing care can access elders monitor data, like heart beat and glucose. It is helpful to doctor when deciding to give the dosage to patient.

No comments:
Post a Comment